Introduction to Gastroshiza
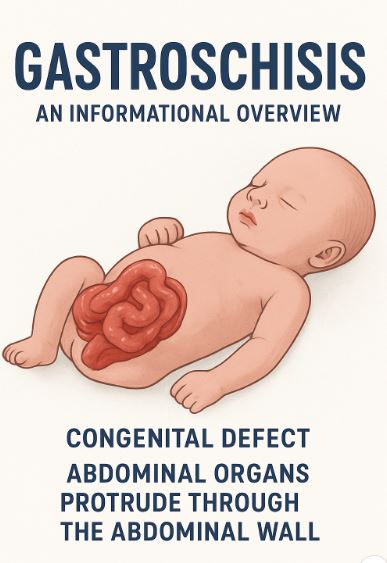
In the world of neonatal medicine, few conditions demand as much urgent attention as Gastroshiza. This rare congenital birth defect involves a baby being born with intestines—and sometimes other organs—protruding outside of the abdominal wall. Unlike similar conditions, the exposed organs are not covered by a protective sac, making Gastroshiza both visibly distinct and medically critical.
For parents, the diagnosis can be overwhelming. Questions arise: Why did this happen? How can it be treated? What is my child’s prognosis? In this article, we’ll explore everything you need to know about Gastroshiza—from causes and symptoms to treatment options, long-term outlooks, and family support.
By the end, you’ll gain a comprehensive understanding of this condition, empowering you with accurate information and resources.
What Is Gastroshiza?
Gastroshiza (sometimes written as Gastroschisis) is a congenital anomaly where the baby’s abdominal wall fails to form properly during fetal development. As a result, the intestines protrude through an opening near the umbilicus (belly button).
Key characteristics include:
- A defect usually located just to the right of the umbilical cord.
- Organs outside the body are unprotected and exposed to amniotic fluid.
- Most commonly, only intestines are affected, but in severe cases, the liver or stomach may also be involved.
Because of the absence of protective covering, infants with Gastroshiza are at high risk for dehydration, infection, and damage to the exposed intestines. Immediate medical care and surgery are essential.
Causes and Risk Factors of Gastroshiza
Genetic and Environmental Influences
While research is ongoing, doctors believe that Gastroshiza results from a combination of genetic, developmental, and environmental factors. Unlike some birth defects, it rarely runs in families, meaning it is typically sporadic.
Common Risk Factors:
- Maternal Age: Women under 20 are statistically more likely to give birth to infants with Gastroshiza.
- Substance Exposure: Use of tobacco, alcohol, or recreational drugs during pregnancy increases the risk.
- Nutritional Deficiency: Poor prenatal nutrition, especially lack of folic acid, may play a role.
- Environmental Toxins: Exposure to pesticides, chemicals, or certain medications during pregnancy is linked to higher incidence.
- Socioeconomic Factors: Limited access to prenatal care and medical resources can contribute to late detection.
How Gastroshiza Differs from Similar Conditions
A common source of confusion is between Gastroshiza and Omphalocele, another abdominal wall defect.
- Gastroshiza: Organs protrude freely without a protective sac.
- Omphalocele: Organs are contained within a thin, transparent sac attached to the umbilical cord.
This distinction is important because Gastroshiza often presents with fewer associated birth defects compared to Omphalocele, but the exposed organs make it more vulnerable to immediate complications.
Symptoms and Diagnosis
Symptoms at Birth
- Visible intestines or organs outside the abdominal wall.
- Red, inflamed, or swollen appearance of the exposed tissues.
- Difficulty maintaining body temperature and hydration.
Prenatal Diagnosis
Thanks to advancements in prenatal care, most cases of Gastroshiza are detected during routine ultrasounds between 18–20 weeks of pregnancy.
Diagnostic methods include:
- Ultrasound Imaging: Detects the abnormality early in pregnancy.
- Amniocentesis (in rare cases): May be recommended to rule out other chromosomal conditions.
Early diagnosis allows doctors and families to plan for immediate surgical intervention after delivery.
Complications Associated with Gastroshiza
Without timely treatment, Gastroshiza can lead to life-threatening complications:
- Dehydration: Because intestines are exposed, fluid loss is significant.
- Infection: Direct contact with bacteria raises the risk of sepsis.
- Intestinal Malfunction: Twisting, swelling, or narrowing of the intestines can cause feeding and absorption issues.
- Short Bowel Syndrome: In rare cases, damaged intestines must be removed, leading to long-term digestive challenges.
Treatment Options for Gastroshiza
Immediate Postnatal Care
Right after birth, neonatal teams take urgent measures:
- Cover exposed organs with sterile, warm, moist dressings.
- Place a protective plastic silo or bag to reduce infection risk.
- Provide IV fluids to prevent dehydration.
- Monitor breathing and temperature stability.
Surgical Repair
Surgery is the definitive treatment for Gastroshiza. The approach depends on the size of the abdominal defect:
- Primary Repair:
- If the defect is small, surgeons return the intestines to the abdomen in one operation and close the abdominal wall.
- Staged Repair (using a silo):
- For larger defects, organs are gradually moved back into the abdominal cavity over several days or weeks.
- Once complete, the abdominal wall is closed.
Post-surgery, infants may need time to adjust before they can digest milk or formula normally.
Prognosis and Long-Term Outcomes
Thanks to advances in neonatal surgery and intensive care, the survival rate for Gastroshiza now exceeds 90% in developed countries.
Short-Term Outcomes
- Most babies recover fully after surgical correction.
- Hospital stays can last several weeks depending on complications.
Long-Term Considerations
- Some children may experience digestive issues or feeding difficulties.
- In rare cases, growth and development may be slightly delayed.
- Ongoing medical follow-ups help track nutrition and gastrointestinal function.
Preventive Measures and Maternal Health
While not all cases are preventable, expectant mothers can lower risks by:
- Maintaining a healthy prenatal diet rich in folic acid and essential nutrients.
- Avoiding smoking, alcohol, and recreational drugs.
- Limiting exposure to harmful chemicals.
- Attending regular prenatal checkups for early detection.
Supporting Families and Resources
A Gastroshiza diagnosis can feel overwhelming, but families are not alone. Multidisciplinary care teams—including surgeons, neonatologists, nurses, and nutritionists—guide parents through the journey.
Support Options:
- Parent Support Groups: Online and local communities provide shared experiences and encouragement.
- Counseling Services: Mental health support helps parents cope with stress and anxiety.
- Educational Resources: Hospitals and nonprofit organizations often offer guides to prepare families for surgery and recovery.
Frequently Asked Questions (FAQ)
1. Is Gastroshiza genetic?
Most cases are not inherited and occur sporadically.
2. Can Gastroshiza be detected before birth?
Yes, usually during the second-trimester ultrasound.
3. How serious is Gastroshiza?
While it is a serious condition requiring immediate surgery, survival rates are very high with modern care.
4. Will my child live a normal life after surgery?
In most cases, yes. Children grow up healthy, though some may face minor digestive challenges.
5. Can Gastroshiza be prevented?
Not completely, but maternal health choices—such as avoiding toxins and maintaining proper nutrition—may reduce risks.
Conclusion: Understanding Gastroshiza in Today’s Medical World
Gastroshiza may be a rare and alarming condition, but thanks to early detection, surgical innovation, and improved neonatal care, the outlook for affected infants is highly positive. Parents can take comfort in knowing that with the right support and medical guidance, most babies go on to thrive and live healthy, fulfilling lives.
Awareness, education, and community support remain vital. By learning more about Gastroshiza, families and caregivers not only gain peace of mind but also help reduce stigma and fear surrounding congenital conditions.
In the end, Gastroshiza is not just a medical challenge—it is a testament to the power of modern medicine, resilience of families, and the hope that every child deserves the best start in life.
Also Read: Kirby Dedo: The Meme, The Legend, and Its Place in Gaming Culture
[…] Explained: Origins, Nutrition, and Delicious Uses Gastroshiza: Causes, Treatment, and Complete Guide for Families Kirby Dedo: The Meme, The Legend, and Its Place in Gaming Culture Premiumindo69: Features, […]
[…] and Everything You Need to Know Tahhiini Explained: Origins, Nutrition, and Delicious Uses Gastroshiza: Causes, Treatment, and Complete Guide for Families Kirby Dedo: The Meme, The Legend, and Its Place in Gaming Culture Premiumindo69: Features, […]